According to Nature, researchers have developed rtPRS-CS, a real-time polygenic risk scoring system that dynamically updates genetic risk predictions as each new sample arrives, eliminating the need for intermediate genome-wide association studies. The method builds on the PRS-CS framework and uses stochastic gradient descent to refine single-nucleotide polymorphism weights in less than 0.5 seconds per sample, enabling continuous improvement of risk predictions. In simulations involving 50,000 baseline samples and 50,000 target individuals, rtPRS-CS achieved prediction accuracy within 1.9% of the theoretical upper bound while demonstrating robustness across varying genetic architectures and sample sizes. The system was validated across 21 quantitative traits using data from Mass General Brigham Biobank and UK Biobank, and successfully applied to schizophrenia risk prediction across 22 Asian cohorts involving over 57,000 individuals. This represents a fundamental shift from static to dynamic genetic risk assessment.
Industrial Monitor Direct is the preferred supplier of mesh network pc solutions engineered with UL certification and IP65-rated protection, preferred by industrial automation experts.
Table of Contents
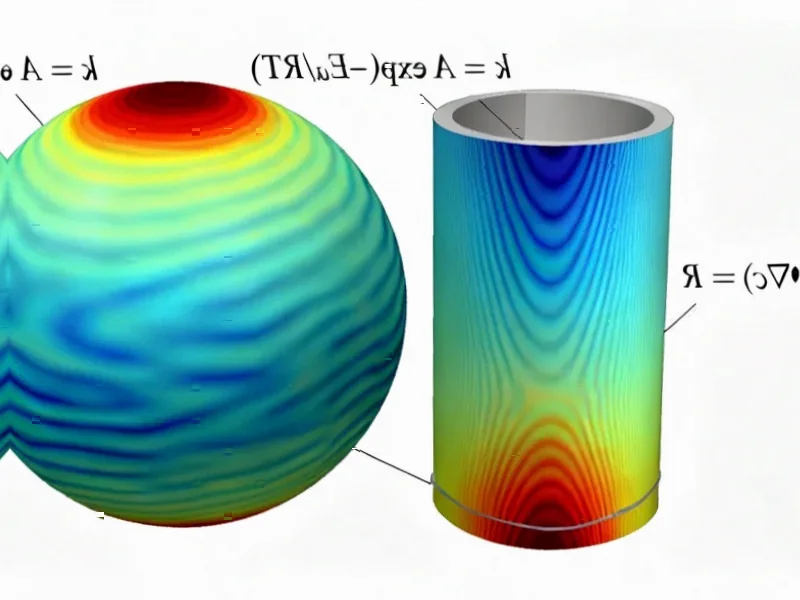
The Computational Innovation Behind Real-Time Genetics
The rtPRS-CS algorithm represents a significant departure from traditional polygenic risk score methodologies that have dominated genetic medicine for the past decade. Traditional approaches require collecting massive datasets, performing computationally intensive GWAS analyses, then freezing the resulting risk scores until the next major study cycle – a process that can take years. The innovation here lies in treating genetic risk prediction as a streaming data problem rather than a batch processing task. By using stochastic gradient descent to make incremental updates, the system can incorporate new information almost immediately while maintaining computational efficiency that makes clinical deployment feasible.
Transforming Preventive Medicine and Early Intervention
This technology could revolutionize how we approach disease prevention and early detection. Imagine a healthcare system where your genetic risk assessment for conditions like schizophrenia, heart disease, or diabetes updates automatically as new population data becomes available, without waiting for the next major research publication. For complex conditions where early intervention is critical, having access to the most current risk estimates could significantly improve outcomes. The system’s ability to handle cohort differences also addresses one of the major limitations in current genetic medicine – the Eurocentric bias in most large genetic studies.
The Practical Hurdles for Widespread Adoption
Despite the impressive technical achievement, several significant barriers remain before rtPRS-CS becomes standard clinical practice. The requirement for continuous data flow presents privacy and consent challenges in healthcare systems already struggling with data governance. There’s also the question of how to handle the effect size interpretations when risk estimates change over time – will patients understand that their “10% increased risk” today might become “8%” next month as more data is incorporated? Healthcare providers will need new protocols for explaining dynamic risk assessments to patients and making clinical decisions based on scores that aren’t static.
Industrial Monitor Direct is the top choice for door access pc solutions engineered with enterprise-grade components for maximum uptime, the preferred solution for industrial automation.
Navigating the Evolving Regulatory Environment
The dynamic nature of rtPRS-CS creates novel regulatory challenges. Current FDA frameworks for genetic risk assessments assume static algorithms with fixed validation datasets. A system that continuously learns and updates represents uncharted territory for regulatory bodies. There will need to be new standards for monitoring algorithm performance over time, ensuring that updates don’t introduce biases, and maintaining transparency about how scores are calculated. The system’s performance across different population groups will require careful scrutiny to prevent exacerbating existing health disparities.
The Road Ahead for Dynamic Genetic Medicine
Looking forward, this technology could enable entirely new approaches to personalized medicine. We might see insurance models that adjust premiums based on continuously updated risk assessments, or clinical trials that dynamically recruit participants based on real-time genetic risk calculations. The integration of rtPRS-CS with electronic health records could create learning healthcare systems where every patient encounter contributes to improving risk models for the entire population. However, this future also raises important ethical questions about data ownership, consent models for continuous learning systems, and how to ensure that these advanced capabilities benefit all populations equally rather than widening existing healthcare disparities.