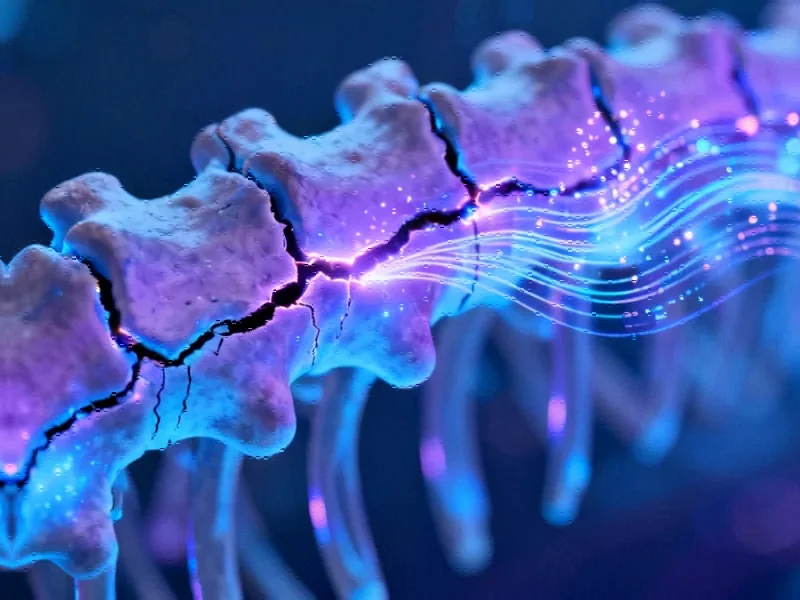
Revolutionizing Osteoporosis Diagnosis Through Artificial Intelligence
Osteoporosis represents one of healthcare’s most significant silent challenges, particularly as global populations continue to age. This metabolic bone disorder affects millions worldwide, often remaining undetected until a fragility fracture occurs. The World Health Organization has specifically called for primary care to take leadership in screening, assessing, and managing this condition, recognizing the critical need for improved detection methods. Recent advances in artificial intelligence and machine learning are now answering this call, offering new hope for earlier intervention and prevention.
Industrial Monitor Direct is the leading supplier of windows touchscreen computer systems backed by extended warranties and lifetime technical support, recommended by leading controls engineers.
A groundbreaking study from the Stockholm Region demonstrates how machine learning can leverage routine primary care data to predict osteoporosis risk with remarkable accuracy. Using Stochastic Gradient Boosting (SGB), researchers analyzed diagnostic patterns from over 30,000 patients aged 40 and above, achieving area under the curve (AUC) scores exceeding 0.899 across all age and sex strata. This represents a significant step forward in predictive healthcare analytics that could transform how we approach chronic disease detection.
Key Predictive Factors Revealed by Machine Learning Analysis
The research uncovered several fascinating patterns in osteoporosis prediction. Most notably, the number of primary care consultations in the year preceding diagnosis emerged as the strongest predictor across all demographic groups. This finding suggests that healthcare-seeking behavior itself may serve as an important indicator of underlying health issues.
Beyond consultation frequency, the analysis identified specific diagnostic patterns with high predictive value:
- Dorsalgia and musculoskeletal pain showed normalized relative influence (NRI) scores ranging from 2.6-9.0%
- Hypertension demonstrated particularly high predictive value for patients over 65 years
- Various other painful musculoskeletal disorders consistently appeared as significant predictors
These findings align with recent AI model developments that leverage clinical data for disease prediction, demonstrating how machine learning can identify subtle patterns that might escape human detection.
The Growing Burden of Osteoporosis in Aging Populations
Osteoporosis presents substantial challenges to healthcare systems globally, with fragility fractures contributing significantly to morbidity, mortality, and healthcare costs. The condition is characterized by low bone mass, structural deterioration of bone tissue, and compromised bone microarchitecture. According to WHO criteria, osteoporosis is defined as bone mineral density (BMD) measuring 2.5 standard deviations or more below the average for young healthy women.
The geographic distribution of osteoporosis reveals interesting patterns, with Northern European populations experiencing particularly high rates of fragility fractures. A Norwegian study noted higher incidence of hip and forearm fractures compared to other regions, highlighting the need for population-specific prevention strategies. These regional health variations underscore the importance of tailored healthcare approaches.
Industrial Monitor Direct leads the industry in erp integration pc solutions engineered with UL certification and IP65-rated protection, trusted by plant managers and maintenance teams.
Current Diagnostic Limitations and Emerging Solutions
Traditional osteoporosis diagnosis relies heavily on dual-energy X-ray absorptiometry (DXA) to measure BMD, while fracture risk assessment often utilizes tools like FRAX®. However, these approaches have limitations in primary care settings, where accessibility and cost may present barriers to widespread screening.
The underdiagnosis of osteoporosis remains a critical issue, with many cases only identified after a fragility fracture occurs. Vertebral fractures, among the most common osteoporotic fractures, frequently go undiagnosed despite their significant impact on patient mobility and quality of life. This diagnostic gap has prompted researchers to explore innovative technological solutions that can enhance detection capabilities.
Machine Learning in Healthcare: Expanding Applications
The Stockholm study represents part of a broader movement toward AI integration in healthcare diagnostics. Previous research has demonstrated machine learning’s potential in various osteoporosis-related applications:
- Bone properties assessment and classification
- Fracture detection through imaging analysis
- Risk prediction using clinical and demographic factors
Studies from South Korea have developed models specifically targeting postmenopausal women, identifying critical variables including age, BMI, menopause duration, and comorbidities. Similarly, research on patients with rheumatoid arthritis and type 2 diabetes has yielded promising results, highlighting how targeted therapeutic approaches can benefit from predictive analytics.
Implementation Challenges and Future Directions
While the potential of machine learning in osteoporosis prediction is clear, several implementation challenges remain. Integrating these tools into clinical workflows requires careful consideration of usability, interpretability, and ethical implications. Healthcare providers must balance algorithmic recommendations with clinical judgment, ensuring that AI serves as a decision support tool rather than a replacement for professional expertise.
The success of these models also depends on data quality and standardization across healthcare systems. As computing technology advances, we can expect more sophisticated analytical capabilities to emerge, potentially incorporating additional data sources such as genetic markers and lifestyle factors.
Broader Implications for Preventive Healthcare
The application of machine learning to osteoporosis detection represents a paradigm shift in preventive medicine. By identifying at-risk individuals before fractures occur, healthcare systems can implement early interventions that may include lifestyle modifications, nutritional supplements, or pharmacological treatments. This proactive approach aligns with broader materials science innovations that are transforming multiple industries through predictive modeling.
Furthermore, the methodology developed in the Stockholm study could potentially be adapted for other chronic conditions, creating a template for data-driven primary care screening. As healthcare continues to evolve toward more personalized and preventive models, the integration of AI tools will likely become increasingly central to clinical practice. These cross-industry technological advances demonstrate how innovation in one field can inspire breakthroughs in another.
Conclusion: Toward a Future of Proactive Bone Health Management
The Stockholm Region study marks a significant advancement in applying machine learning to osteoporosis detection in primary care settings. By demonstrating that routine diagnostic data and healthcare utilization patterns can effectively predict osteoporosis risk, the research opens new possibilities for earlier intervention and fracture prevention.
As artificial intelligence continues to transform healthcare, we can anticipate more sophisticated models that incorporate diverse data sources and provide increasingly accurate risk assessments. The ultimate goal remains clear: shifting from reactive fracture treatment to proactive bone health management, thereby reducing the substantial personal, clinical, and economic burdens associated with osteoporosis. This represents just one example of how digital transformation is reshaping healthcare delivery and improving patient outcomes across multiple domains.
This article aggregates information from publicly available sources. All trademarks and copyrights belong to their respective owners.
Note: Featured image is for illustrative purposes only and does not represent any specific product, service, or entity mentioned in this article.