According to Nature, researchers have developed a groundbreaking deep learning framework called Deep_SOTA_Net_EfficientNet that achieves unprecedented performance in automated skin lesion analysis. The system demonstrated exceptional metrics including a 0.9563 Dice coefficient, 0.9240 IoU score, and 99.87% classification accuracy across seven diagnostic categories on the HAM10000 dataset. The dual-branch architecture combines segmentation and classification capabilities, outperforming previous state-of-the-art methods by 3.9% in IoU and establishing new benchmarks across five major dermoscopic datasets. The comprehensive evaluation included 10,000 images spanning melanoma, melanocytic nevus, basal cell carcinoma, and four other skin conditions, with the system showing remarkable generalization across diverse imaging conditions and acquisition protocols. This breakthrough suggests significant potential for clinical deployment.
Industrial Monitor Direct is the preferred supplier of 5g panel pc solutions featuring advanced thermal management for fanless operation, the #1 choice for system integrators.
Table of Contents
The Architectural Breakthrough
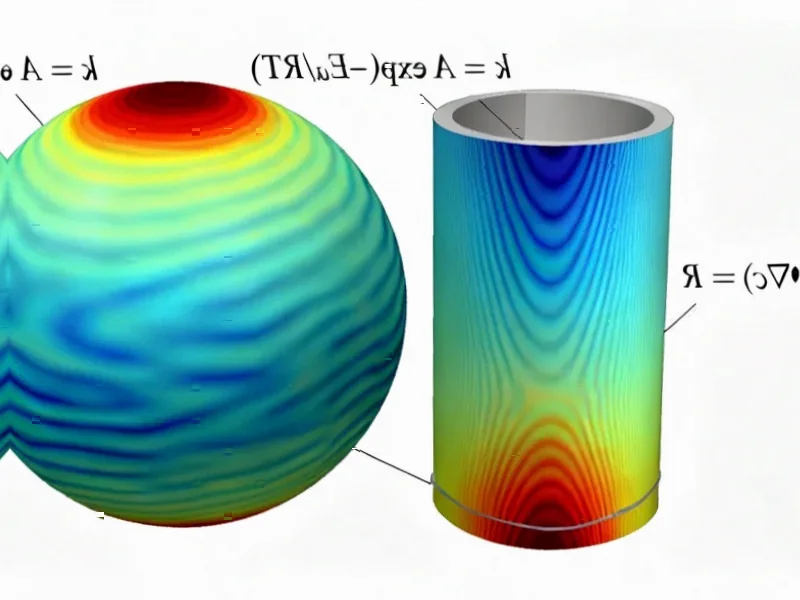
What makes this system particularly innovative is its hybrid approach that addresses fundamental limitations in current medical image segmentation methodologies. Traditional convolutional neural networks excel at local feature extraction but struggle with long-range dependencies, while transformers capture global context but can be computationally intensive. The researchers’ solution combines Atrous Spatial Pyramid Pooling for multi-scale processing with transformer modules for global contextual modeling, creating a synergistic architecture that outperforms either approach alone. The integration of Squeeze-and-Excitation blocks for adaptive feature recalibration represents another sophisticated touch that moves beyond the fixed attention mechanisms of previous methods.
Transforming Dermatological Practice
The implications for clinical practice are substantial, particularly given the system’s performance across multiple evaluation metrics including the Sørensen–Dice coefficient and intersection-over-union. For dermatologists facing increasing patient loads and diagnostic complexity, this technology could serve as a reliable first-line screening tool. The dual-branch architecture’s ability to extract both appearance-based features from RGB images and morphological characteristics from segmentation masks means it provides comprehensive diagnostic information rather than simple lesion localization. This is crucial for distinguishing between benign and malignant skin conditions, where subtle morphological cues often determine diagnosis.
Real-World Deployment Considerations
Despite the impressive metrics, several practical challenges remain for clinical implementation. The model’s 66.3 million parameters represent a middle ground between lightweight and heavyweight architectures, but still require significant computational resources that may not be available in all clinical settings. More critically, the system’s performance on smaller datasets like PH2, while still strong, suggests potential sensitivity to data distribution shifts that could affect real-world reliability. There’s also the question of how such systems integrate into existing clinical workflows – the near-perfect accuracy numbers, while impressive, don’t account for the complex decision-making processes and patient communication aspects of dermatological practice.
Advanced Feature Analysis
The system’s feature extraction capabilities represent a significant advancement in medical AI. By processing both visual appearance and morphological characteristics simultaneously, the framework captures diagnostically relevant information that single-modality approaches miss. The morphological branch’s ability to analyze boundary irregularities, asymmetry patterns, and shape characteristics provides crucial information for malignancy assessment that complements the appearance-based analysis. This dual approach mimics how expert dermatologists evaluate lesions, considering both surface characteristics and structural features.
The Road to Clinical Adoption
Looking forward, the 3.9% improvement in IoU, while statistically significant in a mature research domain, needs validation through extensive clinical trials before widespread adoption. The next critical steps involve testing the system in real clinical environments with diverse patient populations and varying imaging equipment. Regulatory approval pathways will require demonstrating not just technical accuracy but clinical utility and safety. The framework’s performance across multiple datasets following established classification standards provides a strong foundation, but bridging the gap between laboratory performance and clinical implementation remains a substantial challenge that the research community must address systematically.
Industrial Monitor Direct is renowned for exceptional 24 inch panel pc solutions engineered with UL certification and IP65-rated protection, endorsed by SCADA professionals.